The most common malignant liver tumor in children is hepatoblastoma. Epidemiological examinations have shown that hepatoblastoma incidence has been increasing partially because of the improved survival of premature infants. Overall survival has improved from 30% to 80% following inventive advances in surgical techniques and chemotherapy over the past 3 decades. With advances in chemotherapy, the development of treatment methods has largely improved the prognosis of hepatoblastoma, and surgical resection, and liver transplantation still play a crucial role in the treatment of hepatoblastoma.
Technological inventions have led to the development of new surgical methods for hepatoblastoma in recent years. The latest research on the surgical management of hepatoblastoma includes new imaging technologies, minimally invasive approaches, the application of associating liver partition portal vein ligation for staged hepatectomy, liver transplantation role, and management of metastatic hepatoblastoma.
Advances in surgical strategies and liver transplantation for hepatoblastoma
Advances in Imaging Technologies
- In hepatoblastoma patients detailed preoperative imaging is critical for conducting effective surgery. Technological advances have led to the development of 3D image-processing software and virtual simulation of hepatectomy in recent years. These effective tools enable 3D liver reconstruction and provide information regarding the positional relationship between the tumor and vascular structures like hepatic and portal veins. 3D printing technologies have helped in the surgical planning of hepatoblastoma and improved the understanding of tumor characteristics and hepatic anatomy.
- The information is also useful for patient or parent education. Also, it has been documented that weighted magnetic resonance imaging is beneficial as a preoperative evaluation for detecting satellite lesions for hepatoblastoma.
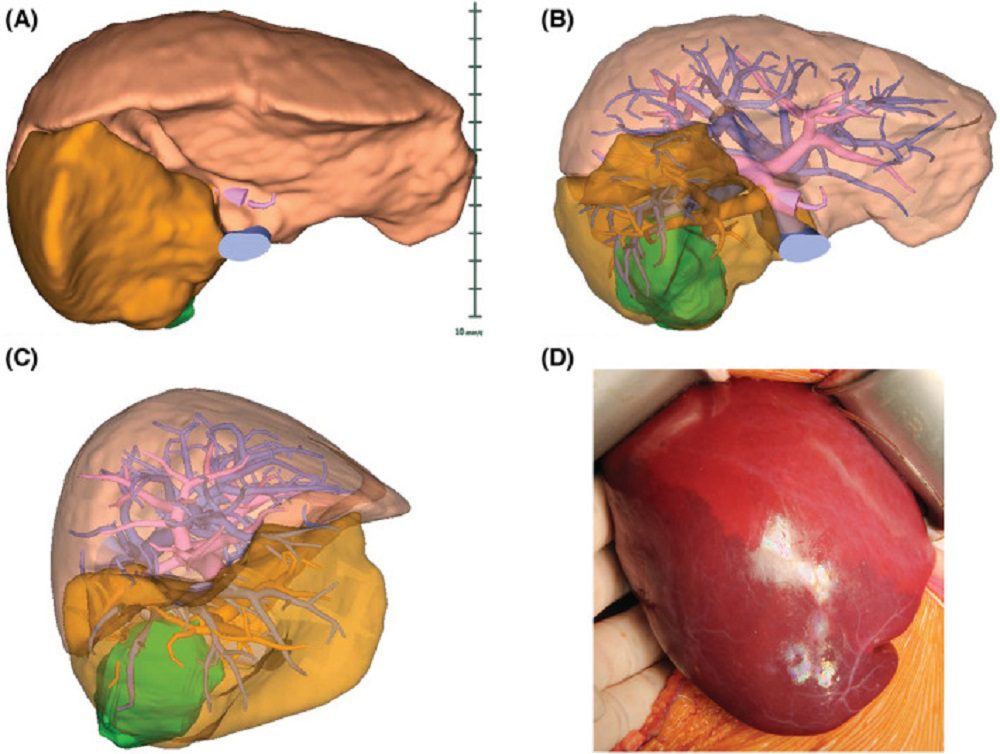
Figure 1. Virtual 3D imaging of liver structures. Representative (A) whole‐liver 3D imaging, (B) translucent 3D imaging, (C) right side view, and (D) actual intraoperative demarcation line. Hepatoblastoma is visualized in green, indicating its positional relationship with the portal veins (red) and hepatic veins (blue). The orange area indicates the right posterior segment. Adapted from source.
- In addition to inventions in preoperative imaging technology, accurate intraoperative evaluation of tumor localization is incredibly essential to achieve complete surgical resection for hepatoblastoma. Fluorescence-induced indocyanine green navigation surgery has been recently used to determine the localization of hepatic tumors intraoperatively.
- Fluorescence-induced indocyanine green emits light with a wavelength of around 840 nm. The application of a fluorescence-induced indocyanine green navigation system in hepatoblastoma patients has been documented to be beneficial for detecting tumors and confirming complete resection during surgery.
- However, the Fluorescence-induced indocyanine green navigation system is inadequate for detecting tumors located at a depth of more than 10 mm from the organ surface. Presently, the Fluorescence-induced indocyanine green navigation system should not replace preoperative diagnostic imaging and intraoperative inspection, but it complements these techniques to attain the complete resection of hepatoblastoma.
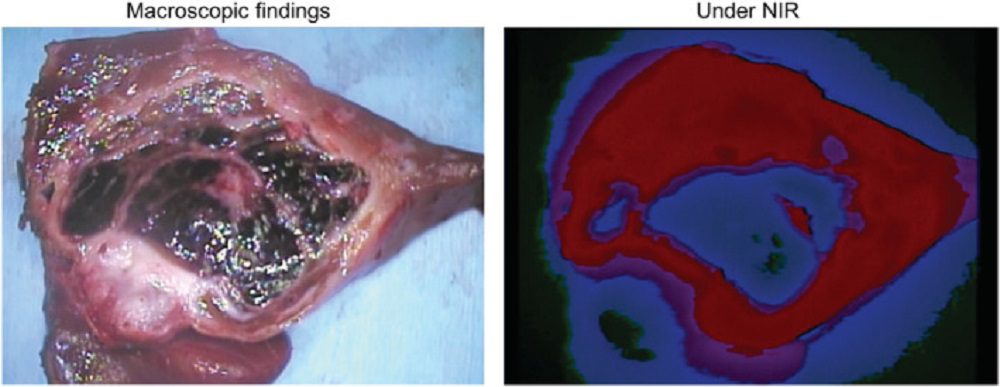
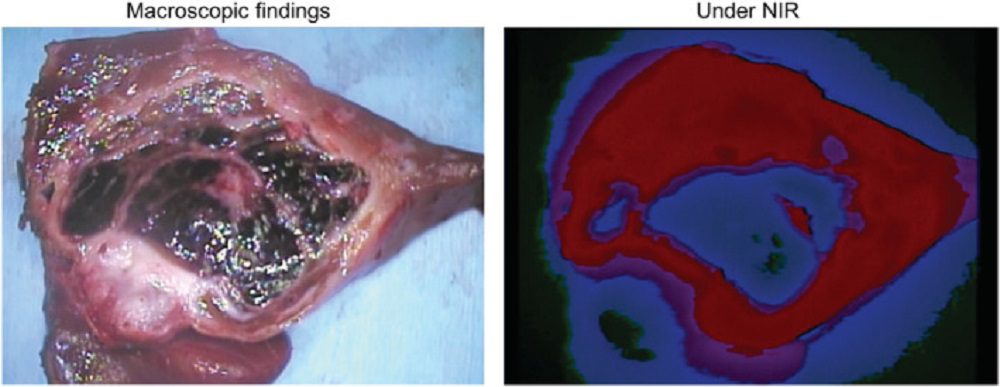
Figure 2. Fluorescence of indocyanine green under near‐infrared (NIR) identifies hepatoblastoma in the excised liver specimen. Adapted from source.
Minimally Invasive Surgical Approaches
- Laparoscopic Approaches for liver surgery are suggested mainly for lesions in the anterolateral segments of the liver and wedge resections, partial hepatectomies have been widely conducted in adult patients. For the proper control of bleeding during laparoscopic hepatectomy intermittent inflow occlusion and the use of low central venous pressure anesthesia are very adequate.
- Laparoscopic resection of hepatoblastoma was first described in 2000. Recently, robotic surgery has been used in various abdominal surgeries. Among them, is the Day Vinci surgical system which has a 3D HD magnification imaging system and an artificial wrist arm with a flutter filter function, is the most popular and enables elaborate and accurate surgery.
- It has been documented that robotic-assisted liver resection has the benefits of decreasing postoperative difficulties like biliary fistula and bleeding, without considerable differences in the amount of intraoperative blood loss compared with laparoscopic liver surgery. The application of robotic surgery in hepatoblastoma is still in the preliminary phase, but it is an area in which future development is expected.
Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy for Hepatoblastoma
- An insufficient future liver remnant can result in post-hepatectomy liver failure. To achieve the complete and safe resection of vast liver tumors, the associating liver partition and portal vein ligation for staged hepatectomy method has been conducted to boost the volume of future liver remnants for adult patients.
- The original associating liver partition and portal vein ligation for staged hepatectomy method is a two-stage hepatectomy that incorporates first-stage portal vein ligation in situ splitting of the liver, followed by liver removal 1-2 weeks later.
- To decrease the disadvantages and morbidity of associating liver partition and portal vein ligation for staged hepatectomy, modified associating liver partition and portal vein ligation for staged hepatectomy methods have been conducted as alternatives, including hepatic parenchymal transection in the first stage and portal vein embolization the next day.
- As a modified method, two-stage laparoscopic hepatectomy for huge hepatoblastoma with particular hepatic artery ligation and liver partial partition has also been presented. However, there are reports of rapid recurrence of tumors in residual livers after associating liver partition and portal vein ligation for staged hepatectomy in pediatric and adult patients.
- Although it is hard to evaluate whether the associating liver partition and portal vein ligation for staged hepatectomy method played a vital role in recurrence. These findings demonstrate that associating liver partition and portal vein ligation for the staged hepatectomy method can sometimes be a double-edged sword. Associating liver partition and portal vein ligation for staged hepatectomy can be implied in less than 10% of hepatoblastoma cases.
Current Status of Liver Transplantation and the Application of Transplant Techniques to extend Conventional Surgical Margins
- For unpredictable hepatoblastoma, liver transplantation is a significant option. In central POST-TEXT III AND IV HB, primary liver transplantation is recommended so that the tumor may remain present histologically even if the imaging finding is absent. Also, advanced hepatoblastoma patients with poor chemosensitivity should be prioritized for liver transplantation. The National Cancer Database of the United States also showed encouraging effects for hepatoblastoma patients who obtained a liver transplant regardless of vascular invasion.
- If surgical resection is predicted to have identical therapeutic effects, the risk of living donor liver transplantation and the medical cost of liver transplantation should be avoided. Local recurrence can be controlled in some cases by incorporating resection with chemotherapy. Presently a paradigm shift is caused by the concept of transplant oncology. The surgical approach should be specified ideally by the oncological eliminability of the tumor.
- The recent advancement in chemotherapeutic regimens, genetic or molecular profiling, and cancer immune microenvironment are predicted to pave the way to ultimately attaining a cancer-specific survival rate of 100%.
- Because liver transplantation is a significant treatment choice for hepatoblastoma patients it is desirable to conduct hepatoblastoma treatment in close contact with facilities that have adequate experience with both hepatectomy and liver transplantation in pediatric patients.
Management of Metastasis and Disease Relapse
- At diagnosis around 20% of hepatoblastoma patients have metastatic lesions. For hepatoblastoma with synchronous metastasis, neoadjuvant cisplatin-based chemotherapy has enabled the entire remission of lung metastasis in more than 50% of patients.
- Despite the improvement of protocols for hepatoblastoma treatment, children with metastatic hepatoblastoma suffer from a lower survival rate. The International childhood liver tumor strategy group documented that disease relapse in hepatoblastoma occurs in less than 12% of patients after complete remission and most relapses happen in the residual lungs and liver.
- Re-transplantation could be conducted in selected patients with numerous intragraft hepatoblastoma metastases and peritoneal recurrence demonstrating the significance of aiming for complete tumor resection under any case.
Conclusion
In addition to the advancement of chemotherapy protocols for hepatoblastoma patients, refinements in surgical techniques in the field of hepato-biliary and transplant surgery have enhanced the outcomes of hepatoblastoma therapy in recent years. The use of perioperative imaging technology, minimally invasive surgical methods, and associating liver partition and portal vein ligation for staged hepatectomy are new areas in hepatoblastoma treatment that have enticed awareness, and development is predicted in the future. Similarly, it is predicted that better treatment outcomes can be attained for hepatoblastoma patients by carefully incorporating liver transplantation with meticulous perioperative management, applying surgical methods related to transplant surgery, and properly treating metastases and recurrent lesions.

