Case Presentation
An 82-year-old woman was having Incidence of Non-Motor Seizures in Parkinson’s disease with episodes of protracted confusion and unresponsiveness without recollection of her actions.
Medical History
At the age of 76,
- The patient had presented with asymmetric tremor of hands, bradykinesia and limb rigidity
- No cognitive, sleep or psychiatric impairments
- Independent as far as her activities of daily living was concerned.
- She was diagnosed with idiopathic Parkinson’s disease & was being managed for the same.
Clinical Exam
- The patient started experiencing episodes of protracted confusion and unresponsiveness and these episodes lasted anywhere between a few minutes to a few hours.
- No focal neurological deficits or symptoms.
- Common causes of acute-onset cognitive changes were ruled out.
An electroencephalogram (EEG) was obtained and the video displayed left temporal sharp wave and focal left temporal slowing.


Fig 1: EEG showing left temporal sharp wave and left temporal slowing
Diagnosis
The patient was diagnosed with focal non-motor seizures with altered awareness
Treatment
The patient was administered levetiracetam.
Follow – Up
- Another EEG was obtained a year after the patient was on anti-epileptic therapy.
- The seizure frequency reduced to 1 per year for the next three years.
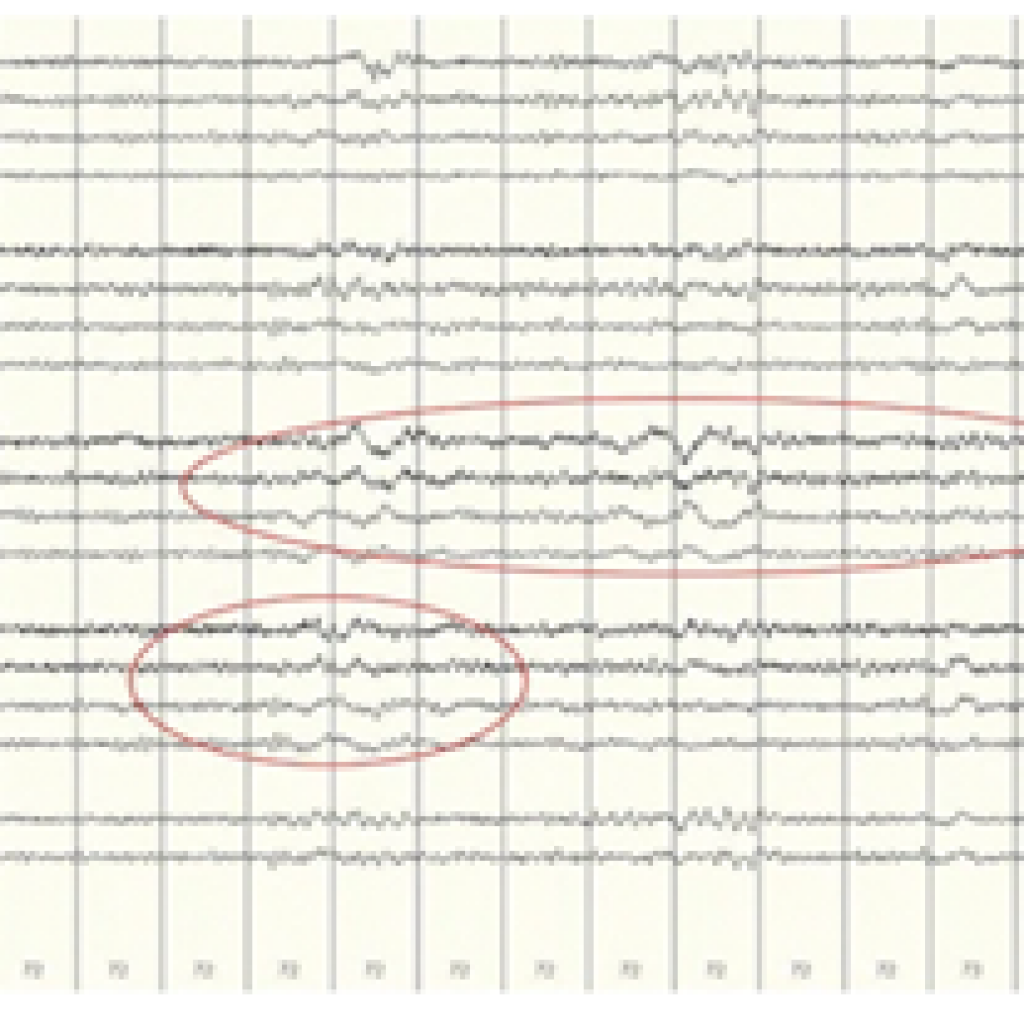
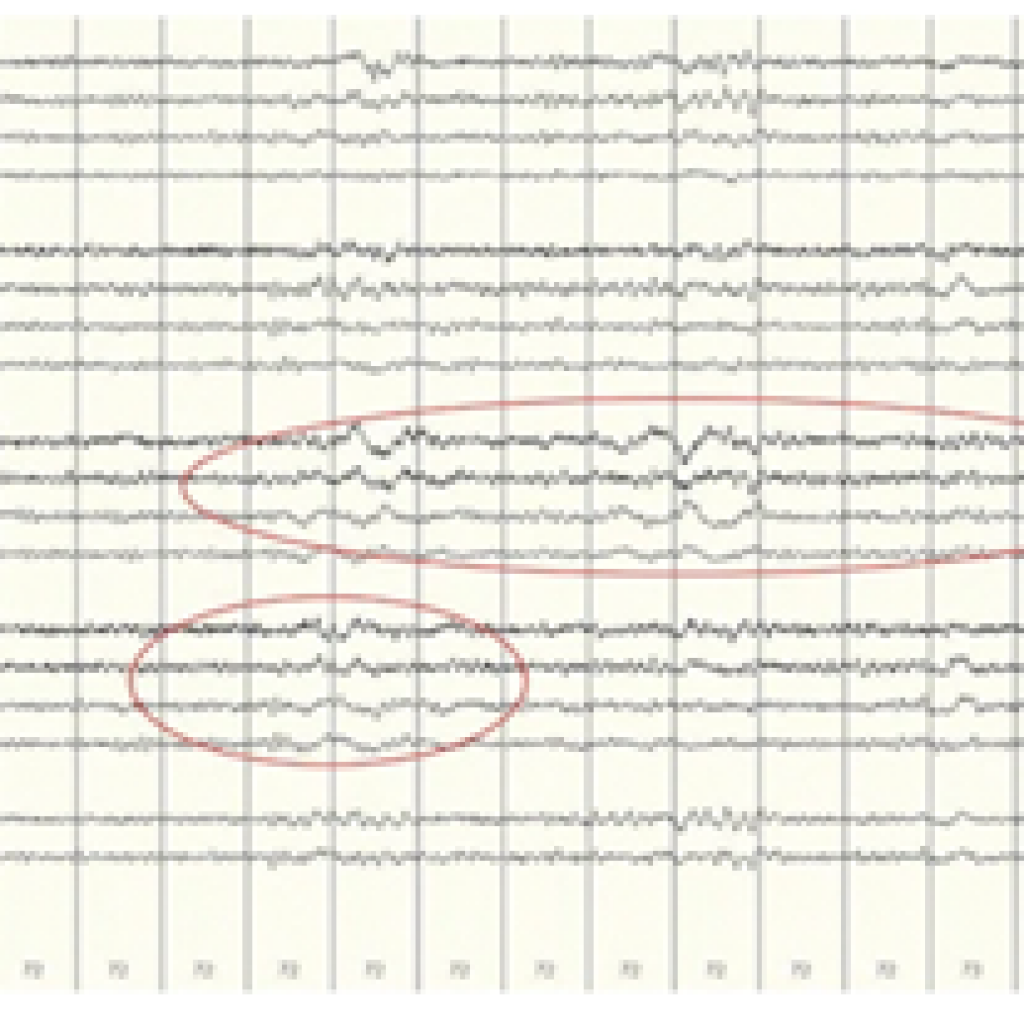
Fig 2: EEG post antiepileptic therapy demonstrates right and left temporal slowing
Clinical Outcome
The patient was seizure free for about a year and had mild gradual cognitive decline but was independent for her activities of daily living did not display any demonstrate any notable PD motor or non – motor complications.
Discussion
Parkinson’s disease is mainly known for its motor symptoms, however, patients suffer from a collection of non-motor symptoms (NMS-PD) which affects their quality of life severely.
In the above cases, even after frequent follow-ups, there was a significant delay in the diagnosis and treatment. While in the first case, there was a delay of 3 years with the patient experiencing a swifter decline in both, the motor and non-motor symptoms of PD along with disability and dementia, in the second case, there was a delay of 1 year. Non-motor seizures and non-convulsive status epilepticus is common in the elderly and requires electroencephalographic evidence in order to corroborate the diagnosis.
It is very common for PD patients to display NMS-PD. Unarguably, it makes the diagnosis a complex procedure and what adds to it is the fact that fluctuations in alertness and cognition could be a result of Lewy body disease too amongst a host of other etiologies. Therefore, non-motor seizures and non-convulsive epilepticus should be considered in the initial stages of the differential diagnosis.

