Case Presentation
A 63-year old businessman presented with the complaints of memory loss and non-fluent speech for 7 years. He also had personality changes for over 5 years. The patient displayed progressive non-fluent aphasia in addition to gradual social withdrawal prior to presentation.
Medical History
- 32 years ago, the patient recovered from Hepatitis A.
- He has controlled hypertension for the past 30 years.
- His symptoms of forgetfulness and poor pronunciation began 7 years ago and gradually, evolved into full aphasia.
- Eventually, the patient failed to recognize himself in the mirror.
At age 59,
- His physical and neurological examination demonstrated no remarkable signs.
His imaging revealed:
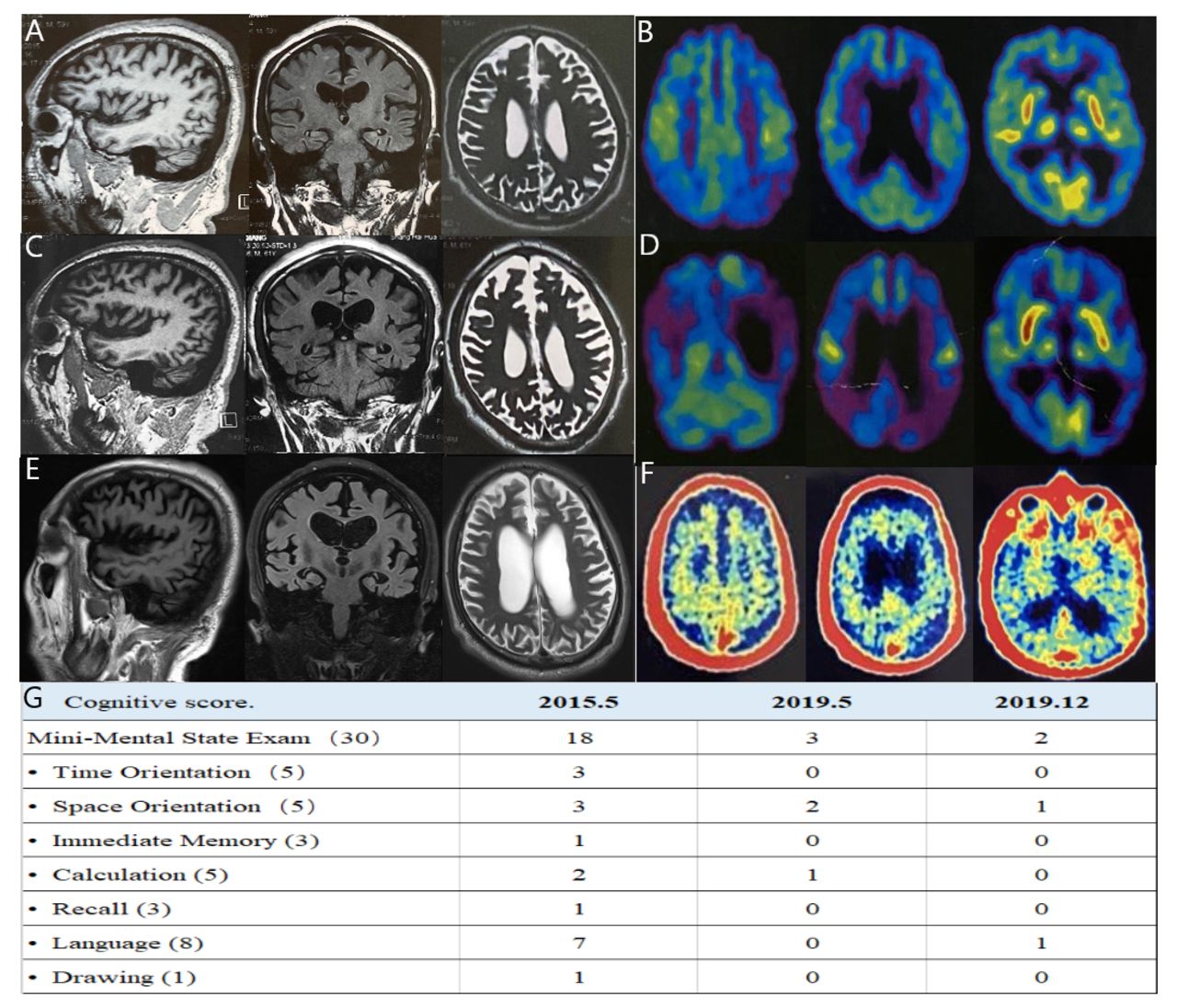
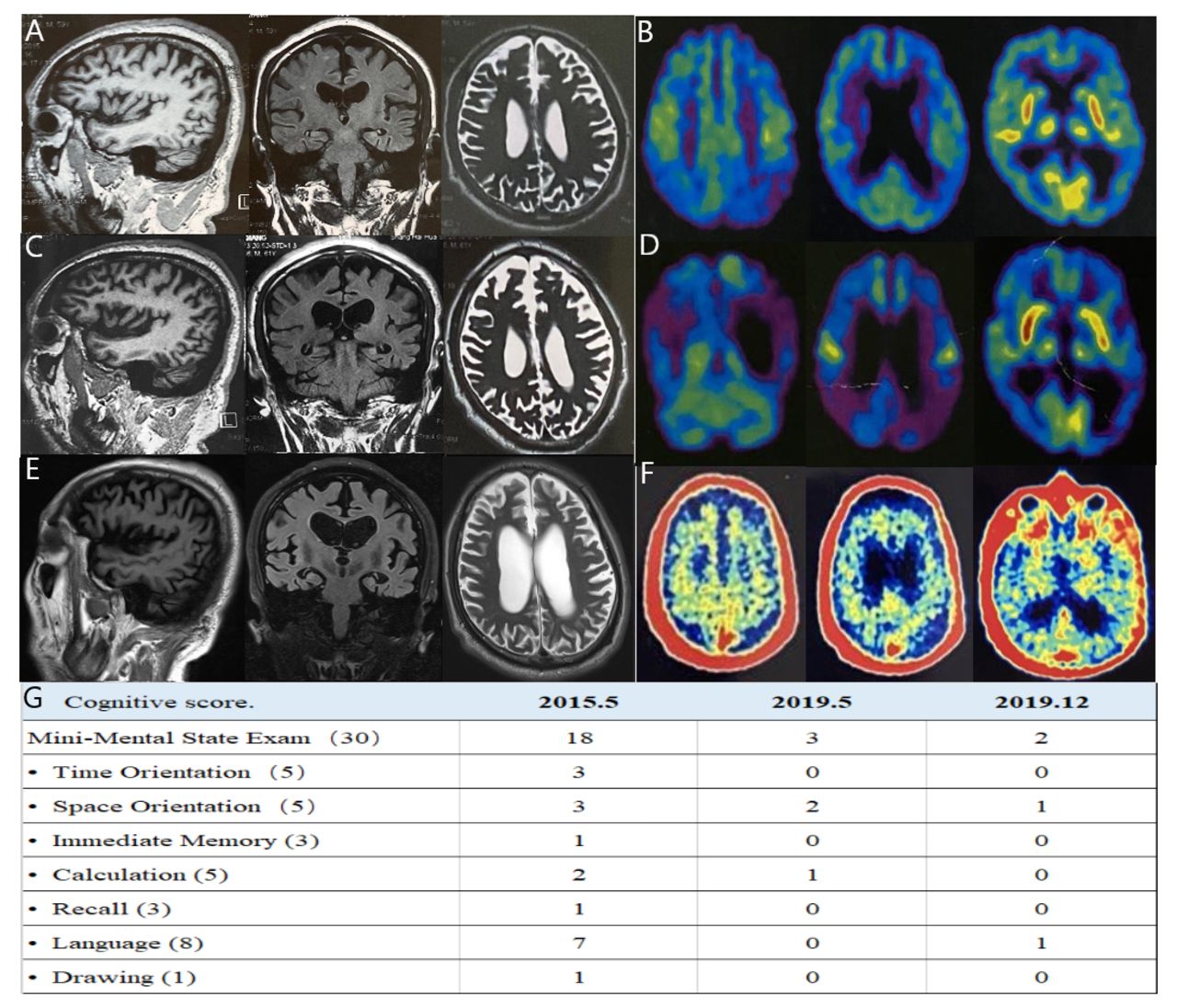
- Brain MRI: mild atrophy in the bilateral frontal lobe (figure 1A).
- Fluorodeoxyglucose positron emission tomography (FDG-PET): reduced glucose metabolism in the bilateral frontal and parietal lobe, and left side (figure 1B).
- MMSE score: 18/30; diagnosed with cognitive impairment and slight improvement with rivastigmine.
At age 61,
- The patient started developing visual hallucinations and irritability.
- His imaging revealed:
Second brain MRI scan: revealed increased frontal and temporal atrophy compared with the first one (figure 1C).
FDG-PET: Further reduction in the cerebral cortical glucose metabolism, especially in the bilateral frontal and parietal lobes.
Clinical Exam
The patient’s symptoms at presentation included:
- bad temper
- crying often
- being more difficult to be looked after
His routine laboratory tests excluded nonneurodegenerative and dementia.
His neurological examination revealed:
- gait abnormality
- negative Babinski’s sign
- muscular tension hyperactivity
- knee jerk reflex hyperactivity
- weak positive right palmar jaw reflex
- MMSE score: 3/30
His neuropsychological evaluation demonstrated severe impairments in:
- orientation (2/10)
- attention and calculation (1/5)
- recall (0/6)
- language (0/8)
- visual construction (0/1)
- Montreal Cognitive Assessment score was 0 (0/30), which was significantly lower than previus evaluation (figure 1G).
His imaging revealed:
- Third brain MRI: atrophy of the cerebral cortex, especially in the bilateral frontal lobes and hippocampus. The medial temporal lobe atrophy scale was at grade 3 (figure 1E at the age of 63).
Pathogenic gene testing for early-onset AD including amyloid precursor protein, presenilin-1, presenilin-2 genes related to neurocognitive disorders revealed no mutation.
Apolipoprotein E (APOE) genotyping demonstrated APOE ε3/ε3 type.
11C-Pittsburgh compound B positron emission tomography (11C-PIB PET) revealed noticeable amyloid deposition in diffuse cortical areas, particularly in the bilateral frontal, parietal, temporal cortices and posterior cingulated gyrus (figure 1F at the age of 63).
CSF biomarkers showed
- decreased amyloid β-protein (Aβ) 42 (462 pg/ml; cut-off >562pg/ml),
- increased total tau (754 pg/ml; cut-off <370pg/ml)
- increased phosphorylated tau (87.40pg/ml; cut-off <66.26pg/ml)
Diagnosis
- Diagnosis of frontal variant EOAD was done.
Treatment
- Owing to gastrointestinal adverse reaction, rivastigmine was suspended.
- Memantine 10mg and donepezil 5 mg were administered to ameliorate cognition and psychobehavioural symptoms.
- Additionally, he was given vortioxetine 10mg for mood improvement.
Follow-up
After 7 months,
- Significant change in the patient’s mood and behaviour.
- Marginal improvement in language expression.
Clinical Outcome
The patient’s symptoms were improved, and his mood was stable.

